Oh no, I have dry eye!
Updated JUN 5, 2023 • 11 min read

Summary in 30 seconds:
In this article, learn more about types of dry eye, symptoms and supportive therapies.
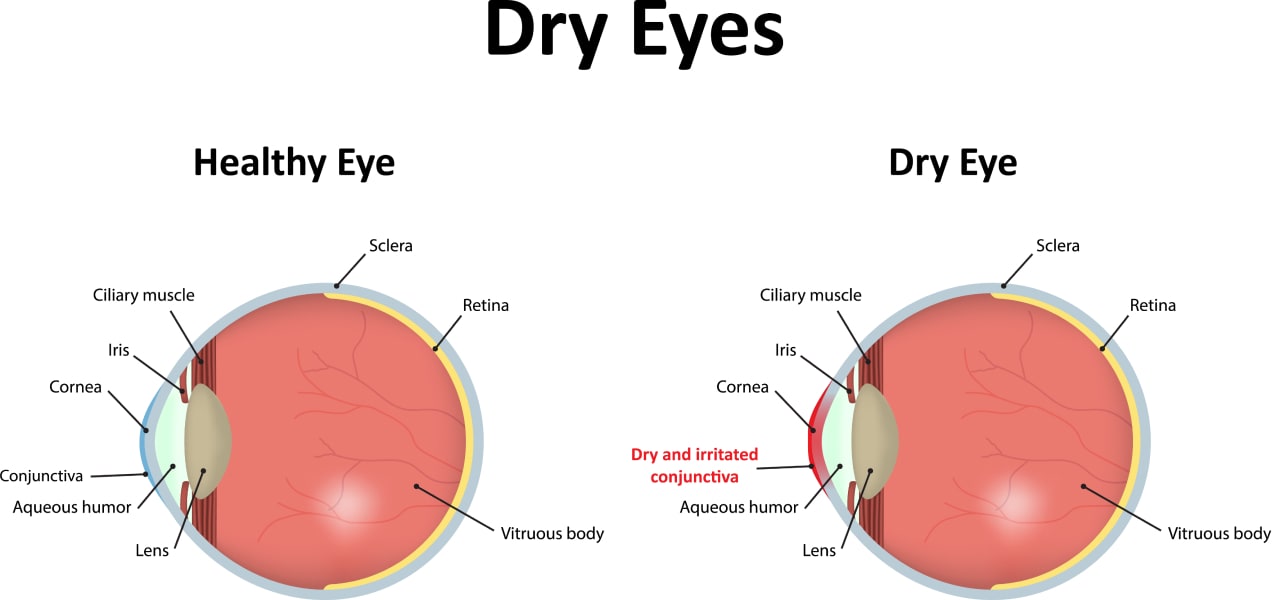
Have you ever experienced symptoms such as your eyes burning, itching, or feeling like there are grains of sand in them? Do you have chronically red, tender irritated eyes? Or, perhaps your eyes “water” all the time. These are very common symptoms of dry eye.
In this article:
- Tears and dry eye
- Basal tears & the tear film
- Types of dry eye
- Medical intervention
- Self-help for dry eye
- Nutritional support for dry eye
Tears and dry eye
Tears play an important role, keeping our eyes comfortable and vision clear. There are three types of tears: basal tears, reflex tears and emotional tears.
- Reflex tears are produced in response to wind, debris or other irritants. These tears act to protect our eyes, wash away debris, and help to fight/prevent infection.
- Emotional tears are released in concert with stress hormones which may be of therapeutic value.
- Basal tears keep our eyes moisturized, nourished and lubricated. Basal tears also help to protect the eyes against infection. In dry eye, it is the quantity and/or the quality of basal tears that are compromised.[1]
Basal tears & the tear film
With each blink, a thin layer of tears is spread over the front surface of the eye. This thin layer is known as the tear film.
A traditional description of the tear film is divided into three layers: an outer oily layer, an inner mucin layer and a watery, aqueous layer in the middle. All three layers work together to help maintain the clarity, comfort, and well being of the surface of the eye.
Disruption of any of these components can lead to ocular surface inflammation, dry eye discomfort and intermittent blurred vision.[2]

Types of dry eye
The cause of dry eye can be broadly categorized into two basic groups: A deficiency in the production of aqueous tears, or their excessive evaporation.
Aqueous tear production deficiency occurs when the lacrimal and accessory glands fail to produce sufficient aqueous tears. [3] Evaporative dry eye occurs when the outer lipid (oily) layer fails to keep the tear film stable allowing excessive evaporation to occur.[4]
Aqueous tear production deficiency: When tear production is inadequate, the ocular surface becomes dehydrated and the tears that are present become overly concentrated. Both prescription and over-the-counter medications may reduce aqueous tears. Examples of these medications include: anti-histamines, beta blockers, sleep aids, diuretics, anti-anxiety medications and pain relievers.
Decreased tear secretion may also be associated with diminished sensitivity of the cornea. This may occur with diabetes, a herpes zoster infection or post ocular surgery. It also may be associated with various autoimmune conditions like rheumatoid arthritis, lupus and Sjogren’s syndrome.[4]
Along with thirst and chapped lips, aqueous deficient dry eye may result from not drinking an adequate amount of water. Ideally, the average person should consume half of their body weight in ounces of water each day.[5]
Evaporative Dry Eye: The function of the outer lipid (oily) layer of the tear film is to help prevent excessive tear evaporation and maintain a stable tear film. This layer is mainly produced and released by glands located in the upper and lower lids known as the meibomian glands.
The healthy function of these glands, and the quality and quantity of meibum oil that they produce is critically important in the prevention of excessive tear evaporation. When the meibomian glands are not functioning properly, it is known as Meibomian Gland Dysfunction (MGD). MGD is the leading cause of dry eye symptoms.
MGD may be associated with the excessive release of lipids and clogging of the glands such as is the case with acne rosacea, allergy, and seborrhea. Scarring of the eyelids may obstruct lipid flow or production. Chronic inflammation of the eyelid margin may also result in scarring. The use of fine powder makeup may plug the meibomian gland ducts reducing the flow of lipid.
No matter the specific cause, disruption of the lipid layer destabilizes the tear film leading to excessive evaporation.[4]
Medical intervention
Dry eye should be evaluated by your eye doctor. Special medical equipment and dyes are used to assess the surface of the eye, eyelids, eyelashes, the tear film and its stability. Additionally, the eyelids need to be checked for complete closure. A dry eye evaluation is often done in conjunction with a regular checkup. Discuss with your doctor regarding any eye drops you may be using.
Systemic conditions and medications may be related to dry eye discomfort. Hormonal imbalances are often associated with dry eye such as during menopause.[6]
Treatment options will depend upon the severity of the dry eye diagnosed and its underlying cause.
Meibomian gland therapies: If you are diagnosed with MGD, discuss the variety of in-office procedures to improve the function of your meibomian glands. These procedures help to unplug the glands and express meibum from the lids.
Artificial tears, gels & ointments: Available over-the-counter, artificial tears are lubricating eye drops designed to soothe dryness and irritation. Some brands of artificial tears mimic natural tears produced by the body. The goal of other brands of tear substitute is to compensate for overly concentrated tears. Oil based artificial tears aim to replenish the lipid layer.

The viscosity (thickness) of various brands of artificial tears ranges from watery to gel to ointment. Gel and ointment formulations cause the vision to blur, so they should only be used before bed. Artificial tears come in preserved and preservative-free formulations. For the greatest benefit, choose an artificial tear designed for your particular needs, activity and time of day. Preservative-free artificial tears are recommended if they are to be instilled frequently such as every hour.
Prescription tear-stimulation eye drops: Tear-stimulation eye drops are designed to increase the production of your own tears. Typically these eye drops are taken twice a day and require a prescription from your doctor.
Punctal occlusion: The puncta is analogous to the drain in a sink. Tears exit the front surface of the eye through a small drainage duct located in the nasal corner of the upper and lower eyelids. The puncta can be blocked temporarily or permanently to allow tears to bathe the front surface of the eye for longer periods of time.
Moisture chambers: Moisture chambers create a high humidity environment which surrounds the eyes. Several designs are available as eyeglasses or wrap glasses, prescription and non-prescription. There are also moisture chamber frames are meant to be worn over your own glasses.[7]
Sleep masks & compresses: There are a variety of masks and moist heat compresses available, including ones that double as a cool compress. Moist heat can be used regularly to help maintain wellness of the meibomian glands. At night, sleep masks provide a humid environment for your eyes and complete eyelid closure.[7]
Nutritional supplementation: Ask your doctor to recommend a dry eye supplement. There are several brands of quality supplements intended to support tear composition and production while reducing inflammation on the ocular surface.
Self-help for dry eye
Environmental modification: Environmental conditions such as wind, forced air heating, air conditioning and blow drying hair can speed up tear evaporation. Running a humidifier helps to increase moisture in the air to help mitigate excessive tear evaporation.
Glasses may help with windy conditions. Avoid smoking or second-hand smoke as smoke is an environmental irritant to the eyes.
Popular Shapes & Styles
Travel: Travel is especially difficult for dry eye sufferers. Whether traveling by car or airplane, plan ahead to proactively modify your environment.
In the car, wear clothing necessary to reduce the need for heat or air conditioning. When flying, apply a drop of artificial tear gel in each eye upon being seated. Wear an eye mask and relax. Your eyes will thank you.
Hydration: Keep well hydrated. Dry eye discomfort and chapped lips are signs of dehydration.
Clean eyelids: Since dry eye can be the result of plugged meibomian gland ducts, practice good eyelid and eyelash hygiene.
Eyelid cleansing decreases the bacterial overgrowth present on the eyelid margin. The exotoxin from this bacterial overgrowth is a common cause of chronic eyelid inflammation (blepharitis) related to MGD dry eye.
Additionally, it is important to be diligent about thoroughly removing eye makeup each day. Makeup, especially mascara and eyeliner, can plug the meibomian gland ducts. Finely powdered mineral makeup may also plug ducts.[8]
Night time dry eye treatment: A great deal of healing occurs during sleep. Part of a nightly routine should include proper lid hygiene. There are products created specially to keep the eyelids makeup free and clean. Before closing your eyes to sleep, put in a gel drop. For severe dry eye, use an ointment or gel formulation of artificial tear and sleep with an eye mask. Your eyes will thank you in the morning.
Both the gel and ointment artificial tears will blur vision but will have all but dissipated by the next morning, sometimes leaving traces on your lids. Clean with a damp face cloth.
Digital device usage: We are constantly using computers, phones, iPads and other devices for work, play and communication. While using these devices, the rate of blinking is often reduced.

Blinking squeezes out tears, then spreads them across the front surface of the eye. Help to keep your eyes moist while working or playing your favorite game by consciously taking a “blinking break.” Blue Light blocking glasses can also be used to help assist and combat digital eye strain.
How to take a “Blinking Break”
This is a modification of the 20/20/20 rule to help with dry eyes associated with digital device usage. This process will take only a minute or two to accomplish. Repeat every half hour , as needed.
- Step 1: Slowly blink 10 times with purpose, closing lids fully. Keep the eyelids closed for 1 – 2 seconds with each blink.
- Step 2: Open your eyes and focus on an object 20 feet away for 20 seconds while blinking normally.
- Step 3: Slowly blink 10 times with purpose closing lids fully. Keep the eyelids closed for 1 – 2 seconds with each blink.
- Step 4: Open your eyes and focus on an object 20 feet away for 20 seconds while blinking normally.
Nutritional support for dry eye.
Modulation of inflammation: No matter the underlying cause of dry eye, the surface of the eye becomes inflamed. Nutritional support of dry eye symptoms is directed at modulating ocular surface inflammation and throughout the body.
To modulate inflammation, it is important to balance dietary intake of the essential nutrients, omega-3 fatty acids with omega-6 fatty acids. For eye wellness, include EPA/DHA omega-3 fatty acids from cold water fatty fish like salmon, barramundi and mackerel.
Limit foods rich in omega-6 fatty acids including vegetable oils and processed foods.[9, 10]
Omega-7 fatty acids: Recent studies show that omega-7 fatty acids found in the pulp and seed oil of Sea Buckthorn improve tear secretion and had anti-inflammatory effects on the ocular surface.[11] Besides Sea Buckthorn, omega-7 is found in macadamia nut oil.
Gut health: Amazingly about 70% of the body’s immune system complex lives within and around the GI tract. To support the composition of the gut flora include probiotic and prebiotic foods such as kimchi, garlic and onions; and foods rich in dietary fiber like raspberries, avocados and artichokes.
Vitamins & phytonutrients: The nutrients in plants with anti-inflammatory and antioxidant properties are known as phytonutrients.
Vitamin D also offers immune support. When exposed to UV-B rays from the sun, the skin produces vitamin D. Mushrooms will also produce vitamin D when placed gill side towards the sun for 30 minutes. The mushrooms may be cooked over medium heat without any harm to the vitamin D.
The EGCGs in green tea support ocular surface wellness. Also, include these nutritional powerhouses in your eye wellness diet: turmeric, ginger, paprika, herbs and spices.
Blood sugar regulation: One symptom experienced by those with diabetes is dry eye. Make sure to follow the advice of your diabetes doctor. Well controlled blood sugar goes beyond dry eye symptoms; it supports the health of the retinal blood vessels inside of the eye.
Published February 9, 2023|Updated June 5, 2023
SOURCES

Related articles

What are Cataracts?
What Are Cataracts – What Are the Main Causes and Cataract Surgery Information

Why Pregnancy and Vision Changes Go Hand-in-Hand
Read on to find out the more common reasons for vision changes in pregnancy

Why Are My Eyes Red?
Why are my eyes red? Reasons your eyes might be red and tips to keep them healthy.


 Tortoise Shell
Tortoise Shell
 Aviator
Aviator
 Full Frames
Full Frames
 Square
Square
 Pink
Pink
 Clear
Clear
 Oversized
Oversized
 Wayfarer
Wayfarer
 Cat Eye
Cat Eye
 Round
Round