What is diabetic retinopathy?
Updated JUN 5, 2023 • 10 min read

Summary in 30 seconds:
In this article we take a deep dive into diabetes, its symptoms, focus on diabetic retinopathy and its effects on vision, as well as relevant treatment options.
In this article:
- The Rise of Diabetes
- What does food have to do with it?
- What is diabetes?
- Types of diabetes
- What are the symptoms of diabetes?
- Risk factors for developing diabetes & diabetic retinopathy
- Treatment options for diabetic retinopathy
The rise of diabetes.
Diabetes and pre-diabetes affect millions of Americans. According to CDC data 37.3 million have diabetes and 96 million are estimated to have pre-diabetes. Over the past 20 years the prevalence has significantly increased (2001 – 2020). [1,2]
As diabetes increases, so do ocular complications from diabetic retinopathy; it is the leading cause of visual impairment in the working-aged adult population in the US. [3]
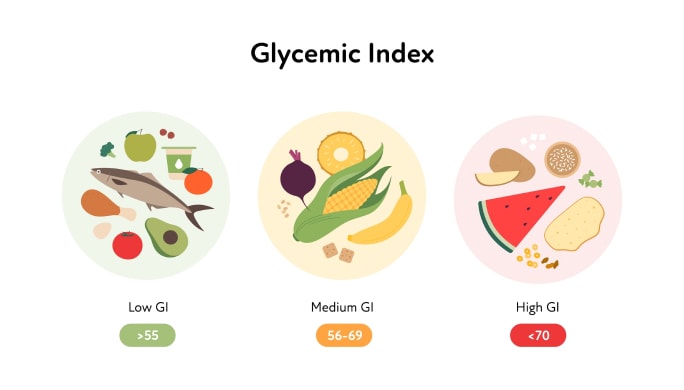
What does food have to do with it?
The food we eat and drink provides energy for the body to function. The major nutritional components of food are known as macronutrients: proteins, lipids and carbohydrates. Each of these macronutrients contributes to overall health and wellness.
Protein-rich foods include: fish, meat, eggs, beans, nuts and tofu. Lipids are fats like olive oil, vegetable oils and butter. Examples of foods that are rich in carbohydrates include: fruit, potatoes, grains and sugar.
The body processes and utilizes each of the macronutrients differently. When carbohydrates are consumed, the body breaks them down into a sugar known as glucose; it is then released into the bloodstream.
Unlike carbohydrates, fats and proteins have little influence on blood glucose levels when they are metabolized. [4] Although in diabetes, the body’s response to the consumption of protein may be altered. [5]
Insulin, the key to the cell’s door
Glucose provides fuel for cells throughout the body and it is the main source of energy for the brain. In order for the body to utilize glucose, the hormone insulin is needed. Insulin is like a key that opens the door of a cell to allow glucose to enter.
Insulin is produced by beta cells in the pancreas. Beta cells respond to the presence of glucose in the bloodstream by releasing insulin.
For good health, blood sugar levels should remain within a target range. And, the cells in the body need to be able to respond appropriately to insulin.
So, what is diabetes?
In diabetes, insulin production and/or its utilization are out of balance in response to blood glucose levels. Without adequate insulin, glucose remains in the bloodstream.
Elevated blood glucose damages blood vessels in the eyes and throughout the body. Areas of the body with small capillary beds are first affected.
Chronically elevated blood glucose increases the risk for cardiovascular disease, kidney disease, nerve damage and eye disease known as diabetic retinopathy. [6,7,8]
Types of diabetes:
- Type 1: Type 1 diabetes is an autoimmune disease process that destroys beta cells in the pancreas. This results in deficient insulin production. Both children and adults are affected by Type 1 diabetes; it can occur at any age.
Often children are diagnosed in early elementary school or during puberty and growth spurts associated with hormonal changes. Only 5 – 10% of diabetes cases are Type 1. [9] - Type 2: Type 2 diabetes develops over time. Insulin is still produced by the pancreas but the cells in the body are increasingly less responsive to it. Glucose in the blood then remains higher for a longer period of time because insulin is less effective at allowing glucose to enter cells.
To compensate, even more insulin is produced. Eventually the insulin producing cells burn out and are not able to meet the body’s requirements. - Gestational diabetes: The body during pregnancy can have difficulty producing sufficient insulin, especially during the second and third trimesters. There are many hormones released during pregnancy, some which encourage weight gain. This can then lead to insulin resistance.
If insulin resistance was present prior to pregnancy, gestational diabetes is more likely to occur. It is important to monitor blood glucose during pregnancy because gestational diabetes increases the risk for high blood pressure and complications of childbirth. [10]
What are the symptoms of diabetes?
Symptom presentation of type 1 diabetes may take months or even years to develop. Before enough beta cells in the pancreas are destroyed, there may be no noticeable problems. Once noticed, symptoms can be severe. [9]
Type 2 diabetes begins gradually. At first, there is insulin resistance then later, once the pancreas no longer releases sufficient insulin, as full blown type 2 diabetes. The diagnosis of type 2 diabetes may be delayed because symptoms may go unnoticed for years.
Increased thirst & urination: Glucose is normally reabsorbed by the kidneys to be used again. But when there is more glucose than can be reabsorbed, more fluid is required to flush out the excess glucose. This leads to symptoms of increased thirst and frequent urination especially at night.
Dry eyes & blurry vision: Since the body is using extra fluid for excretion other areas become dry including your eyes and skin. Also, the lens inside of the eye can swell leading to blurry vision. These symptoms may be intermittent.
Fatigue and hunger: Glucose provides energy to cells. When glucose is not able to enter cells due to insulin resistance or a lack of insulin, fatigue and hunger may result.
Other symptoms of diabetes include: unexplained weight loss, sores that heal slowly, more infections than usual, and tingling in the hands or feet.
Risk factors for developing diabetes & diabetic retinopathy
According to the CDC, [11,12] risk factors for diabetes and retinopathy include:
Type 1 diabetes risk factors: A close family member with type 1 diabetes such as a sibling or parent. While type1 diabetes can develop at any age, children, teens and young adults are at a higher risk.
Type 2 diabetes risk factors: Currently have pre-diabetes; overweight; more than 45 years old; have a parent or sibling with type 2 diabetes; physically active less than 3 times per week; non-alcoholic fatty liver disease; gestational diabetes; polycystic ovary syndrome; race/ethnicity – African American, Hispanic descent, American Indian, Native Alaskan, Asian descent.
Gestational diabetes: Pregnancy increases the risk of developing retinopathy in women who were diagnosed with diabetes prior to pregnancy and those who develop gestational diabetes during pregnancy.
Diabetic retinopathy risk factors: Having any type of diabetes is a risk factor for developing diabetic retinopathy. The longer a person has diabetes the greater the chance of developing diabetic retinopathy, especially if diabetes has been present longer than 10 years.
Poor blood sugar control and diabetic kidney disease increases the likelihood for developing retinopathy. There is an association between high blood pressure, serum lipids and the development of retinopathy. [13]
How does diabetic retinopathy affect the eye?
Elevated blood glucose damages the tiny blood vessels that support the retina. The retina is the light sensitive lining inside the back of the eye. The damaged blood vessels are weakened leading to swelling, fluid leakage and small hemorrhages. Small bulges in the vessels can develop.
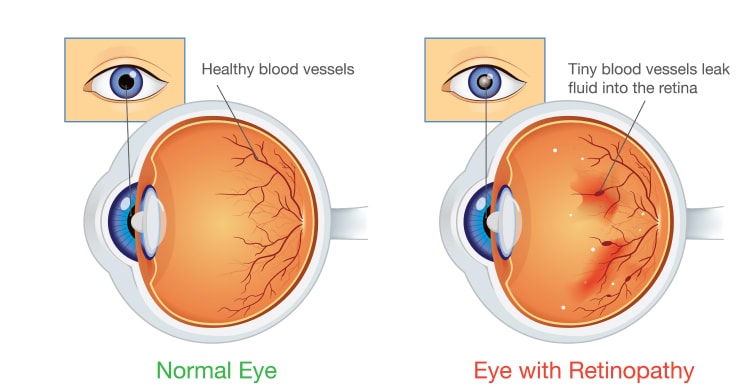
Sometimes vessels close and deprive the retina of oxygen. In response new, fragile blood vessels begin to grow in the retina and into the gel in front of the retina. Bleeding from these fragile vessels may cause vision to become cloudy. Swelling from fluid leakage may affect the macula.
The macula is responsible for seeing details clearly and for color vision. Vision loss is often related to fluid accumulation, bleeding and/or scarring of the macula. This damage can occur elsewhere in the retina. Diabetic eye disease may result in cataract formation, retinal detachment and even glaucoma.
The two main stages of diabetic retinopathy are NPDR (non-proliferative diabetic retinopathy) and PDR (proliferative diabetic retinopathy)
NPDR (non-proliferative diabetic retinopathy): NPDR is an early stage of diabetic eye disease. There may be mild or no symptoms. Distortion of blood vessels and tiny hemorrhages may be noted upon examination by your eye doctor.
At this stage, these vessels swell and leak fluid. Decreased vision is often not present unless there is swelling in the macula.
PDR (proliferative diabetic retinopathy): PDR is a more advanced stage of retinopathy. Damage to the retina accumulates over time. In response to the lack of oxygen, new fragile blood vessels grow onto the surface of the retina.
These vessels break and bleed into the gel like fluid in front of the retina. The bleeding can then progress to fibrous scarring; damage to the retinal cells; traction on the retina; retinal detachment; and, ultimately severe vision loss.
Treatment options for diabetic retinopathy
Treatment options for diabetic retinopathy depend upon the stage of the retinopathy, symptoms, general health and age.
Laser surgery: A laser can be used to seal leakage of blood and fluids. It is also used to reduce retinal swelling and discourage new blood vessel growth.
Vitrectomy: The vitreous is a clear gel-like fluid in front of the retina. If bleeding into the vitreous occurs, vision may be blocked. A vitrectomy removes the cloudy vitreous and replaces it with a balanced saline solution.
Ocular injections: An anti-VEGF (Anti-Vascular Endothelial Growth Factor) medication may be injected into the eye. These injections are especially helpful for patients suffering vision loss due to swelling in the macula.
Good diabetes control
Here are a some tips to help maintain good diabetes control:
- Follow the advice of your diabetes doctor. Healthy habits and lifestyle are important to the management of diabetes. Follow the dietary recommendation given to you by your diabetes doctor. Your diabetes doctor may suggest nutritional counseling tailored to your individual requirements.
- Blood glucose levels, blood pressure and blood lipids need to be monitored regularly. To assess the health of your eyes, a dilated eye examination is necessary upon a diagnosis of diabetes and regular visits thereafter per your eye doctor’s recommendation.
Special ophthalmic equipment is used to evaluate the condition of the retina and internal ocular structures. Frequently there are no symptoms of diabetic eye disease until it has progressed to an advanced stage. - Support your cardiovascular wellness through maintaining a healthy weight, regular exercise, not smoking, adequate sleep, manage stress and follow your diabetes doctor’s recommendations.
Published January 15, 2023|Updated June 5, 2023
SOURCES

Related articles

What are Cataracts?
What Are Cataracts – What Are the Main Causes and Cataract Surgery Information

Why Pregnancy and Vision Changes Go Hand-in-Hand
Read on to find out the more common reasons for vision changes in pregnancy

Why Are My Eyes Red?
Why are my eyes red? Reasons your eyes might be red and tips to keep them healthy.